Acute pancreatitis (AP) has many attainable etiologies and hypertriglyceridemia (HTG) accounts for up to 10{fe463f59fb70c5c01486843be1d66c13e664ed3ae921464fa884afebcc0ffe6c} of all conditions [1,2]. In 15-20{fe463f59fb70c5c01486843be1d66c13e664ed3ae921464fa884afebcc0ffe6c} of instances of critical HTG, usually outlined as triglyceride levels higher than 1000 mg/dL, development to AP may well come about [2].
The precise mechanisms by which HTG induces pancreatitis are not recognized and varied theories have been purposed, together with the part of genetic, metabolic, and environmental will cause [2,3]. The most approved speculation indicates that the surplus of chylomicrons in circulation leads to occlusion in pancreatic capillaries inducing hydrolysis of these triglyceride-wealthy lipoproteins by pancreatic lipase into no cost fatty acids that direct to toxicity to the pancreatic endothelium and acinar tissue [4]. The hyperviscosity concept hypothesizes that accumulation of chylomicrons in the microcirculation reduces pancreatic capillary blood stream foremost to ischemia [5]. Ultimately, the recognition of genetic polymorphisms as possible danger factors for the improvement of AP elevated the speculation of genetic involvement in the pathogenesis of hypertriglyceridemia-induced pancreatitis (HTG-AP) [3]. Familial HTG may well also lead to HTG-AP and autoantibodies from lipoprotein lipase (LPL) or its regulatory proteins may perhaps trigger obtained chylomicronemia [6].
Apart from the supportive therapy that ought to be presented to all clients with AP, which include intravenous hydration, analgesic medication, and a fastening state, it is significant to think about other therapeutic measures directed to its unique etiology. In the placing of HTG-AP, distinct cure possibilities have been used, these kinds of as heparin, insulin infusion, and plasmapheresis [5]. Infusion of unfractionated heparin releases LPL attached to the endothelial cells, which potential customers to a transient reduction in serum triglycerides [7]. Having said that, there are some dangers associated with this remedy as it leads to depletion of LPL on the surface area of endothelial cells which could guide to a new raise in serum triglycerides [8]. Furthermore, it may boost the hemorrhagic possibility in the location of pancreatic necrosis [9]. Insulin infusion is other commonly utilized tactic as it promotes the synthesis of LPL from adipose and muscle mass cells having said that, there is no distinct evidence of its advantage in non-diabetic individuals. The non-invasive character of therapy with insulin is definitely desirable but calls for watchful checking [2,5].
As mortality linked with HTG-AP could reach 30{fe463f59fb70c5c01486843be1d66c13e664ed3ae921464fa884afebcc0ffe6c}, starting a more aggressive and quickly successful therapy these as plasmapheresis might be justified [6]. Having said that, even in the environment of intensive treatment, HTG-AP is not a popular sign for plasmapheresis [10-12]. In accordance to the very last published pointers on therapeutic apheresis, HTG-AP constitutes an indication of group III (Grade 1C) for therapy with plasmapheresis, that means that the the best possible function of apheresis treatment is not proven and determination-building ought to be individualized [6]. Extracorporeal elimination of large lipoproteins is hypothesized to end more organ damage and it is imagined that plasmapheresis can drastically reduce triglyceride concentrations, cut down inflammatory cytokines, and perhaps switch deficient LPL when fresh frozen plasma (FFP) is utilised as substitution fluid. Reductions in triglyceride amounts of 49-97{fe463f59fb70c5c01486843be1d66c13e664ed3ae921464fa884afebcc0ffe6c} have been noted subsequent a solitary technique. Treatment method aims depend on triglyceride reduction at the very least to moderate-moderate stages, routinely outlined as <500 mg/dL [6]. The main complications associated with plasmapheresis are hypotension, infection, hypersensibility reactions, bleeding, and hypocalcemia [11]. Herein, we present a case of HTG-AP successfully managed with plasmapheresis.
A 38-year-old Asian male with a known history of hyperlipidemia presented in the emergency department with severe abdominal pain that started eight hours before admission. The patient denied any previous history of alcohol consumption or smoking and was not taking any medication. Vital signs at admission were as follows: blood pressure 135/85 mmHg, heart rate 117 beats per minute (bpm), respiratory rate 16 cycles per minute (cpm), and temperature 36.8ºC. Physical examination was positive for umbilical and right lumbar pain. Laboratory workup revealed normal serum amylase and severe HTG of 3170 mg/dL (Table 1).
|
Laboratory results
|
Value
|
Normal range
|
|
Hemoglobin (g/dL)
|
14.4
|
13-18
|
|
Leucocytes (cells/uL)
|
10,400
|
3,800-10,600
|
|
Neutrophils (cells/uL)
|
7,700
|
1,800-6,900
|
|
CRP (mg/dL)
|
2.29
|
<0.3
|
|
Lactate (mmol/L)
|
1.35
|
<1.80
|
|
Platelets (platelets/uL)
|
185
|
150-440
|
|
Amylase (U/L)
|
92.7
|
28-100
|
|
Total cholesterol (mg/dL)
|
567
|
<200
|
|
LDL cholesterol (mg/dL)
|
554
|
<115
|
|
HDL cholesterol (mg/dL)
|
13
|
>55
|
|
Triglycerides (mg/dL)
|
3,170
|
<150
|
|
Glucose (mg/dL)
|
179
|
60-100
|
|
Creatinine (mg/dL)
|
0.91
|
0.70-1.20
|
|
Urea (mg/dL)
|
23.2
|
<50.0
|
|
Calcium (mg/dL)
|
7.3
|
8.6-10.0
|
|
Ionized calcium (mmol/L)
|
1.2
|
1.15-1.35
|
|
Urine glucose
|
++++
|
0
|
An abdominal ultrasound was performed showing hepatic steatosis without other relevant findings. A computed tomography (CT) scan at admission showed globosity of pancreatic tissue and small volume of peri-pancreatic effusion. A diagnosis of HTG-AP was made and the patient was admitted to the gastroenterology ward. Upon the observation of severe HTG without hyperglycemia, it was decided to start treatment with plasmapheresis. A central venous catheter was placed and plasmapheresis treatment was started, using a PrismaFlex® monitor with a TPE 2000® filter (Lund, Sweden: Baxter International Inc.) (Table 2). Anticoagulation was prescribed with unfractionated heparin at a rate of 500 IU/hour.
|
Plasmapheresis prescription
|
|
Filter
|
TPE 2000
|
|
Qb (mL/min)
|
200
|
|
Reposition fluid volume (mL)
|
3000
|
|
Reposition fluid rate (mL/h)
|
800
|
|
Reposition fluid
|
Albumin 5{fe463f59fb70c5c01486843be1d66c13e664ed3ae921464fa884afebcc0ffe6c}
|
|
Treatment duration
|
3 h 45 min
|
|
Anticoagulation
|
UFH
|
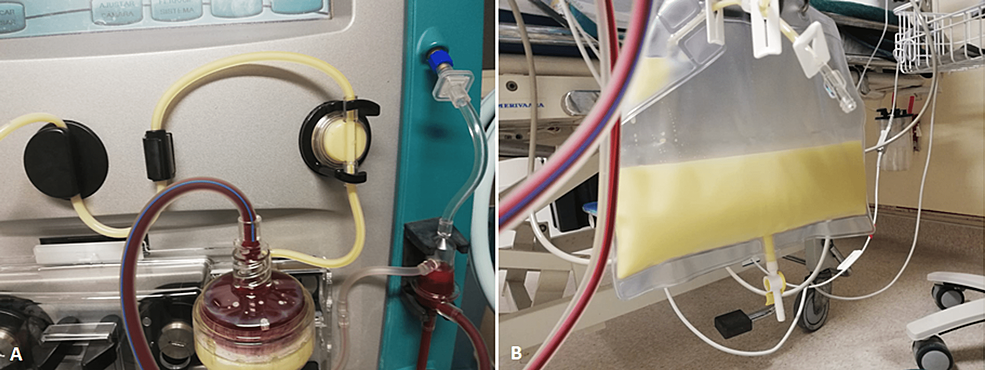
During plasmapheresis treatment, it was possible to document the milky appearance of the filtered plasma in the extracorporeal circuit and in the effluent bag (Figures 1A, 1B). There were no complications associated with the procedure. Approximately 12 h after treatment, the triglyceride levels were under 500 mg/dL, and symptoms progressively remitted. Imaging study by CT scan was repeated after 48 h revealing small areas of necrotic pancreatic tissue and increased volume of peri-pancreatic effusion. After 72 h, liquid diet (per os) was restarted and was well tolerated. During hospitalization, the patient kept blood glucose levels between 140-260 mg/dL and HbA1c was 9.5{fe463f59fb70c5c01486843be1d66c13e664ed3ae921464fa884afebcc0ffe6c} leading to the diagnosis of diabetes mellitus.
Figure
1:
Filtered plasma (A) in the extracorporeal circuit and (B) in the effluent bag during plasmapheresis.
The patient was discharged after one week of hospitalization and referred to endocrinology and gastroenterology consultations under treatment with bezafibrate and atorvastatin. Oral antidiabetic treatment was also started with metformin and sitagliptin. The evolution of triglycerides and total serum cholesterol, low-density lipoproteins (LDL), and high-density lipoproteins (HDL) levels after discharge are shown in Table 3.
|
Lipid profile
|
12 h post-plasmapheresis
|
At discharge
|
After 3 months
|
|
Triglycerides (mg/dL)
|
457
|
521
|
690
|
|
Total cholesterol (mg/dL)
|
130
|
255
|
330
|
|
HDL cholesterol (mg/dL)
|
15
|
NA
|
38
|
|
LDL cholesterol (mg/dL)
|
115
|
NA
|
292
|
There were neither new hospitalizations nor the need for additional plasmapheresis sessions after six months of follow-up. The patient is currently treated with a combination of statin and fibrate, without adverse effects to report and with good lipid control.
HTG-AP may present as a life-threatening condition requiring aggressive treatment to control disease activity. Of note, in this case, amylase levels were always under the threshold of three times the upper limit of normal, as previously described in patients with HTG-AP [13,14]. Lipase measurement would be more specific than amylase for the diagnosis of pancreatitis, but it was not available in the emergency department laboratory panel. In this case, we emphasize the effectiveness of a single treatment with plasmapheresis in the reduction of HTG leading to a favorable outcome, with the first treatment reducing triglyceride levels by 85.6{fe463f59fb70c5c01486843be1d66c13e664ed3ae921464fa884afebcc0ffe6c}. A milky appearance of the effluent is an expected finding, and it is a consequence of the high concentration of triglycerides in the filtered plasma. When available, we think plasmapheresis may be helpful in rapidly decreasing serum triglycerides and stopping the pathogenic pathways of HTG-AP. In this case, the patient had normal blood glucose levels at admission, which supported the decision of not starting insulin perfusion, since plasmapheresis was available as an alternative method. While lowering of triglyceride concentrations in the setting of HTG-AP is achievable with plasmapheresis, it is not known the exact extent of the benefit in terms of overall morbidity and mortality. Despite the marked reduction of HTG levels observed in this patient, the 48 h imaging studies revealed signs of worsening disease with small necrotic pancreatic areas. Although there are no randomized clinical trials showing its superiority compared to other treatments, other reports of the use of plasmapheresis in this clinical setting strongly suggest that it can be a safe and useful option for severe cases [7,15-19].
The Bi-TPAI trial, the first randomized clinical trial that compared insulin therapy to plasmapheresis showed no significant differences between both interventions. However, further studies are needed to elucidate the potential beneficial effects of plasmapheresis in the subgroup of patients with a suboptimal lowering of triglycerides with conservative treatment or patients with a severe course of pancreatitis [20,21].
Regarding long-term follow-up, the type of therapy used to treat pancreatitis seems to have no impact on the control of triglyceride levels. In this case, the patient had re-elevation of triglyceride levels three months after discharge. Knowing that statins and fibrates are two powerful medications against HTG, treatment with n-3 polyunsaturated fatty acids and nicotinic acid may also be considered [22]. In rare cases where triglyceride levels remain uncontrolled despite optimal therapy and pancreatitis recurs, plasmapheresis may be used as prevention treatment [23,24].
HTG-AP may have a severe clinical course with mortality rates as high as 30{fe463f59fb70c5c01486843be1d66c13e664ed3ae921464fa884afebcc0ffe6c} of cases. Different treatment options are available, such as insulin or heparin perfusion, but other therapeutic alternatives should be considered in the setting of severe cases. In this case, a single plasmapheresis session was effective and well-tolerated treatment, without associated complications.
Even if HTG-AP is a rare indication for this technique, plasmapheresis results in early and effective triglyceride reduction. However, large-scale studies are needed to further assess the efficacy of plasmapheresis and to help define subgroups of patients that may have higher benefits from this therapy.